Health insurance coverage for fertility treatments varies widely. Some policies cover specific treatments, while others exclude them entirely.
Understanding health insurance coverage for fertility treatments can be complex. Different insurance plans offer varying levels of coverage for procedures like IVF, IUI, and medications. It’s crucial to review your policy details or speak with a representative to know what is included.
Many factors, such as state laws and employer-specific plans, influence coverage. Knowing your benefits can help you plan financially and emotionally for fertility treatments. Always check for any required pre-authorizations or network restrictions to avoid unexpected costs. Comprehensive knowledge of your insurance plan ensures you make informed decisions about your fertility journey.
Introduction To Fertility Treatments
Fertility treatments have become a beacon of hope for many couples. These treatments help those struggling to conceive naturally. Understanding these procedures is essential for anyone considering them.
Common Procedures
Several common procedures fall under fertility treatments. Here are the most frequently used ones:
- In Vitro Fertilization (IVF): This involves fertilizing an egg outside the body.
- Intrauterine Insemination (IUI): Sperm is directly inserted into the uterus.
- Egg Donation: Eggs from a donor are used for fertilization.
- Sperm Donation: Donor sperm is used for fertilization.
- Surrogacy: Another woman carries and delivers the baby.
Who Needs Them
Fertility treatments are necessary for various individuals and couples. Here are some common reasons:
- Women with Ovulation Disorders: They have irregular or no ovulation.
- Men with Low Sperm Count: They have fewer sperm available for fertilization.
- Couples with Unexplained Infertility: No specific cause is identified.
- Individuals with Genetic Disorders: They want to avoid passing conditions to their child.
- Same-Sex Couples: They need donor eggs or sperm to conceive.
Understanding these treatments helps in making informed decisions. Knowing who needs them can guide many towards the right path.
Credit: www.arcfertility.com
Types Of Health Insurance Plans
Understanding the types of health insurance plans can help determine if fertility treatments are covered. Two main types are Private Insurance and Employer-Sponsored Plans.
Private Insurance
Private insurance plans are bought by individuals. They offer different coverage options. Check if your plan includes fertility treatments. Some plans might cover tests but not treatments. Always read the policy details.
Employer-sponsored Plans
Employer-sponsored plans are provided by employers. They often have better coverage than private plans. Some employers offer plans that include fertility treatments. Ask your HR department about your coverage. They can give you plan details.
| Plan Type | Coverage |
|---|---|
| Private Insurance | Varies, often limited to tests |
| Employer-Sponsored | Varies, often includes treatments |
- Check if fertility treatments are covered.
- Read policy details carefully.
- Ask HR for employer plan details.
Coverage Variability
Understanding health insurance coverage for fertility treatments can be complex. Coverage variability plays a significant role in determining what treatments are covered. The scope of coverage can differ based on several factors. Let’s delve into the main aspects that influence coverage variability.
State Mandates
State mandates significantly impact fertility treatment coverage. Some states require insurance companies to provide coverage for fertility treatments. This ensures that residents in these states have better access to necessary treatments. Here’s a list of states with mandates:
- Massachusetts
- Connecticut
- Illinois
- Maryland
- New Jersey
Each state has its own specific requirements. This means that what is covered in one state may not be in another. Always check your state’s regulations.
Policy Differences
Even within the same state, insurance policies can differ. Companies offer various plans with different levels of coverage. Some plans may cover only basic treatments. Others might offer comprehensive coverage, including advanced procedures like IVF.
Here are some common differences in policies:
| Policy Type | Coverage Details |
|---|---|
| Basic Plan | May cover initial consultations and diagnostic tests. |
| Mid-tier Plan | Includes medications and some treatment cycles. |
| Premium Plan | Offers extensive coverage, including IVF and other advanced treatments. |
Always review your policy documents carefully. Understanding your plan’s specifics can save you from unexpected costs.
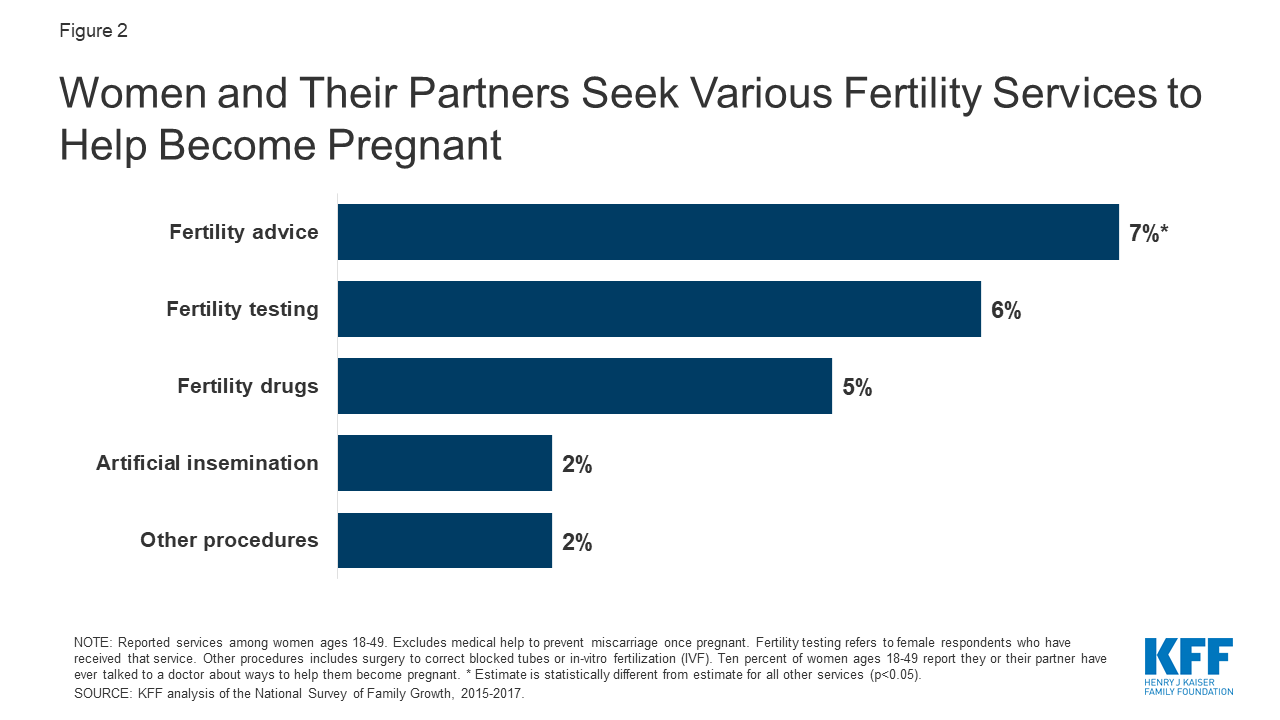
Credit: www.kff.org
Commonly Covered Treatments
Understanding what fertility treatments are covered by health insurance can be confusing. This section breaks down the most commonly covered treatments. Knowing this can help you navigate your journey to parenthood.
Ivf
In vitro fertilization (IVF) is a popular fertility treatment. Many insurance plans cover it. IVF involves combining eggs and sperm outside the body. The embryo is then placed in the uterus. Insurance coverage varies, so check your plan details.
Some plans cover the entire IVF process. Others may only cover parts, like egg retrieval. Make sure you understand what your plan includes. This can save you from unexpected costs.
Medications
Fertility medications are essential for many treatments. These drugs stimulate egg production. They also regulate the menstrual cycle. Many health insurance plans cover these medications.
Common medications include:
- Clomiphene citrate
- Gonadotropins
- Metformin
Check if your insurance covers these drugs. Coverage can vary widely. Some plans may have limits on the number of cycles covered. Always verify the details with your insurance provider.
Injectable medications are also used in fertility treatments. These can be expensive. Insurance may cover these, but the extent of coverage can differ. Always ask for a detailed list of covered medications.
| Medication | Purpose | Typical Coverage |
|---|---|---|
| Clomiphene citrate | Stimulates ovulation | Partially covered |
| Gonadotropins | Stimulates multiple egg production | Varies by plan |
| Metformin | Improves insulin resistance | Often covered |
Out-of-pocket Costs
Understanding the out-of-pocket costs for fertility treatments is crucial. These costs can add up quickly and vary widely. Knowing what to expect can help you plan better.
Deductibles And Copays
Most health insurance plans have deductibles and copays. These are out-of-pocket costs you must pay before your insurance starts to cover expenses.
Deductibles are fixed amounts you pay each year before the insurance kicks in. This means you might have to pay a significant amount upfront.
Copays are smaller, fixed fees you pay for each visit or service. They are usually required for doctor visits, lab tests, and medications.
Financing Options
Fertility treatments can be expensive. Many people use financing options to manage these costs.
Here are some common financing options:
- Personal loans
- Credit cards
- Specialized fertility financing programs
Some clinics offer payment plans. These plans can break the costs into manageable monthly payments.
Below is a table summarizing potential out-of-pocket costs:
| Cost Type | Description |
|---|---|
| Deductible | Annual amount paid before insurance covers costs |
| Copay | Fixed fee for each visit or service |
| Personal Loan | Borrowed money to cover medical expenses |
| Payment Plan | Monthly payments offered by clinics |

Credit: resolve.org
How To Navigate Your Coverage
Navigating health insurance for fertility treatments can be tricky. Understanding your policy and asking the right questions are crucial steps.
Reading Your Policy
Start by reading your health insurance policy thoroughly. Look for sections that mention fertility treatments or reproductive health. Policies often have a table of contents. Use it to find relevant sections quickly.
Next, identify key terms like “in-network”, “out-of-network”, “deductible”, and “copay”. These terms will help you understand what costs you might incur. Some policies cover only specific treatments, such as IVF or IUI. Others might cover consultations but not procedures.
It’s important to note any waiting periods. Some policies require you to wait a certain period before coverage starts. Understanding these details will save you time and money.
Asking The Right Questions
Once you have read your policy, ask your insurance provider the right questions. Here are some essential questions to consider:
- Does the policy cover fertility consultations?
- Are specific treatments like IVF or IUI covered?
- What are the out-of-pocket costs?
- Are there any pre-authorization requirements?
- Is there a limit on the number of treatments covered?
These questions will give you a clear picture of your coverage. Always get the answers in writing. This ensures you have a record for future reference.
Take notes during your call with the insurance provider. Write down the name of the representative you spoke with. Record the date and time of the call. This information could be crucial if disputes arise later.
Knowing your coverage details empowers you to make informed decisions. It helps you plan financially and emotionally for fertility treatments.
Frequently Asked Questions
Does Health Insurance Cover Ivf Treatments?
Some health insurance plans cover IVF treatments. Coverage varies by provider and policy specifics.
Which Fertility Treatments Are Commonly Covered?
Commonly covered treatments include diagnostic tests, medications, and some procedures like IUI. Coverage varies widely.
Can I Appeal A Denied Fertility Claim?
Yes, you can appeal a denied claim. Contact your insurance provider for the appeals process.
Are There Fertility Treatment Coverage Limits?
Yes, many plans have coverage limits. These can include lifetime maximums or limits on the number of cycles.
Is Pre-authorization Required For Fertility Treatments?
Many insurance plans require pre-authorization. Check with your provider to understand the requirements.
Conclusion
Understanding your health insurance policy is crucial for fertility treatment coverage. Policies differ, so research thoroughly. Consult your provider for specific details. This knowledge empowers informed decisions about your reproductive health. Stay proactive and advocate for your needs.